The Epidemic of Immobility

There is an entire senior industry built around preventative measures and responses to protect older people from falling, and with good reason. According to the National Council on Aging Falls Prevention Facts, “falls remain the leading cause of fatal and nonfatal injuries for older Americans.” Aside from grievous and sometimes fatal injuries, falls are costing money, lots of money. In 2015 Medicare and Medicaid paid 75 percent of the 50 billion dollars in total cost due to fall injuries. With an ever-aging US population, the financial toll is projected to reach 67.7 billion dollars in 2020.
The Centers for Medicare and Medicaid Services (CMS) made a declaration that falls should never happen in a hospital environment and created penalties that became effective in 2008. The penalty still allows for patient care billing through CMS but will no longer bump payments up to a higher level to cover the treatment of fall-related issues. The advent of the Affordable Care Act (ACA or “Obamacare”) saw Congress introduce more stringent penalties by reducing federal payments by one percent for those hospitals with the highest rates of falls as well as other hospital-acquired conditions. The financial aspect is of significant concern as the American Hospital Association (AHA) finds that nearly one-third of US hospitals report negative operating margins.
These government assessed fall penalties could damage a hospital’s reputation and reduce its profitability. As a result, many hospital policies are now overzealous with regards to fall prevention, creating an epidemic of patient immobility. While this epidemic may serve the financial interests of hospitals, it does not serve the needs of older hospitalized patients. There are nominal reasons that hospitals are promoting increased “bed rest.” These reasons include a shortage of staff, insufficient walking equipment, and no current means to record ambulation in a patient’s electronic medical record. Some nurses and hospital aides, to evade being reprimanded if a patient under their supervision falls, find reasons to avoid getting a patient out of bed and walking. Patients themselves are being instructed not to get up on their own and are subject to bed alarms that will alert hospital staff if they do.
Elderly patients are bedbound and discouraged from walking. This practice degrades the patient’s mental well being and their ability to become well to protect hospital profitability. Many older patients are weak and frail upon hospital admission, and after a few days in bed, find their muscles can deteriorate significantly enough to bring severe long-term consequences. Dr. Kenneth Covinsky, a researcher and geriatrician at the University of California-San Francisco, states, “Older patients face staggering rates of disability after hospitalizations.” His research cites that one-third of patients age 70 or more leave the hospital more disabled than when they were admitted.
Ultimately the policies put in place to reduce the number of falls in a hospital setting have created a climate of “fear of falling.” Hospital staff feels that a patient falling on their watch will lead to blaming, reprimands, even termination when the fault of the fall might be the patient themselves. This staff self-protection mechanism creates a cycle where the patient languishes in bed, growing weaker by the day. When they do get up, the patient is more likely to fall and become more seriously injured due to a decrease in muscle coordination and an increase in strength deterioration.
Barriers to the mobilization of elderly hospital patients do them a great disservice and may lead to increased length of hospital stay as well as disability after hospitalization. The limiting of patient mobility may have begun as a response to financial penalties but has very serious, though perhaps unintended, patient health consequences. Inpatient walking activity is a good predictor of readmission in elderly Americans. Research shows that just 275 steps a day while in the hospital yields lower rates of readmission after 30 days. Programs such as the Hospital Elder Life Program (HELP) are trying to reduce the barriers to patient mobility and reverse the epidemic of elder patient immobility. Across America, there are efforts to get patients moving again in special hospital wings called Acute Care for Elders. In these specialized settings, elderly patients can be provided the proper staff and equipment to walk and enhance their rehabilitation and wellness safely. For the best elderly patient outcomes, the trend of patient immobility must become less prevalent in hospitals despite the risk of falls.
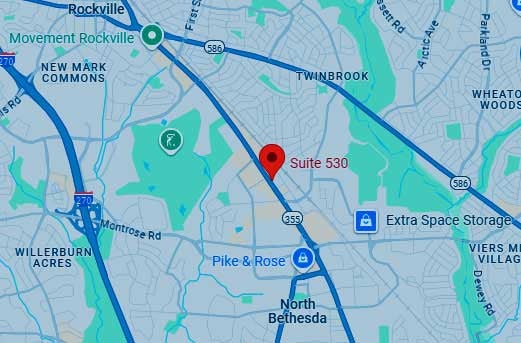
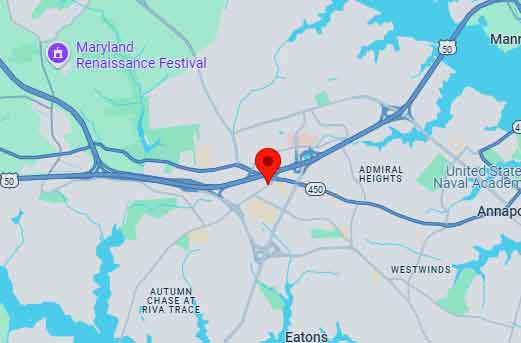
If you have any questions or need guidance in your planning or planning for a loved one, please contact any of our five offices by calling (443) 393-7696.
Understand These Before Turning 65

In the United States, turning 65 years of age is a milestone on many levels, but before this birthday, there is a hefty checklist that you need to address to continue aging successfully. Overall the most crucial thing to do before turning 65 is to invest your time wisely crafting the best approach possible for your health and financial security well-being.
Can you afford to retire? Are you married? Estimate your total annual spending, including a cushion for periodic or unforeseen expenses like home repairs or dental work. Total all of your potential retirement-income sources and understand the tax implications associated with their spending. Run through several scenarios where you change what year you claim social security benefits to see if you should defer collecting it to a later age. Be realistic and start adhering to a modest budget today. Very few Americans can withdraw a lot from personal savings and investments without risking running out of money too soon. As you start to gather your assessments in general about how you view your retirement, find a qualified retirement planning expert that can help you with projections that are based on realistic assumptions.
Familiarize yourself with Medicare and its associated program variations. If you are retiring, you will approach Medicare differently than if you continue to work and have health care available through your employer. If you no longer will have health care through an employer, learn about Medigap supplemental insurance policies as Medicare will not cover all of your health care. Health insurance becomes quite complicated and varies widely depending on your overall health and personal financial situation. The National Council on Aging (NCOA), in partnership with private companies Aon Retiree Health Exchange™ and Via Benefits™, provides a checklist and timeline that can guide you through the process of enrolling in Medicare and assessing how you will cover the cost of prescription medication. If your income is low, you may qualify to enroll in Medicaid, which covers more expenses than Medicare. If you have already begun to take your social security benefits, then you will automatically be enrolled in Medicare. A packet entitled “Welcome to Medicare” will be sent to your address three months before turning 65. There are essential actions to take and deadlines associated with this packet, so read through the material carefully and meet those deadlines.
There are resources available to help you understand what your options are and the best way for you to proceed. As you approach the age of 65 many private insurance companies will lobby for your insurance dollars that will be spent on supplemental insurance. Finding a retirement planning company with insurance brokers that can sell you policies from many different insurance companies is more advantageous than locking into a group that will only sell plans that are associated with their company. A reputable insurance broker should not charge for helping you to assess your situation as they make commissions from the insurance company providing the policy to you. Check with the Better Business Bureau (BBB) online where you can plug in the name of an insurance group or retirement counselor and find out how long they have been in business, their accreditation, BBB rating, and customer reviews and complaints.
If you are over the age of 50, you can contribute an extra 1,000 dollars annually to your IRAs and an additional 6,000 dollars to 401(k)s up until the age of 65, according to Kiplinger. If you are still working, this is an excellent way to boost your retirement spending money. Before 65, you need to explore the option of a long-term care insurance policy, which helps to pay for any assisted living care needs you may require in the future. Long-term care policies can be expensive. If you do not enroll in a long-term care plan before the age of 65, the policies will become practically unaffordable.
Before turning 65, you should also come to terms with your will, advance medical directives, trusts, and the difficult conversation with your spouse or children about your end of life wishes and any funeral arrangements. Take heart, turning 65 is far from a death sentence as many Americans are living long and active lives well beyond the age of 65; however, meeting with an elder counsel attorney can save you and your heirs’ plenty of money and heartache. Do not wait until an adverse medical event forces your family or loved on to act on your behalf financially or medically. Decisions made under duress do not provide the best outcomes. Beyond your will, power of attorney and power of medical attorney, consider a dementia directive as well. Projections for the aging US population indicate an ever-increasing number of seniors who have Alzheimer’s and other forms of dementia. Your elder counsel attorney can guide you through your options. Some states even have working templates for dementia directives. As you age, you can review your legal strategies from time to time and make adjustments as you deem necessary. It isn’t easy to discuss your end of life scenario, but once you have had the discussions and put proper legal documents into place, you can move forward with a sense of relief. It is freeing to make decisions and act on your future behalf, knowing you can always revisit your choices.
Now for the fun stuff; get excited about the senior discount. While it is true that there are discounts available as early as 55 and 62, nothing beats the senior discount at age 65. You can check off that bucket list of yours with deals on restaurant meals and travel excursions, clubs, retail stores, hotels, cinemas, smartphone plans, AARP membership discounts, and more. If you do not see an offering for a 65 senior discount posted, by all means, ask.
Beyond Medicare eligibility, you can get a onetime free physical exam if you have Medicare Part B insurance coverage. Gyms and community programs offer discounted or free physical fitness programs so that you can keep yourself moving and as healthy as possible. If you have Medicare, check out your eligibility for SilverSneakers for a 65+ fitness program. Your local senior center can keep you socially active and connected to people your age. Making friends and enjoying the simple act of conversation is known to have many benefits for your cognition and staves off isolation and depression issues.
If you retire from your job at 65, you can finally begin to collect on your pension plan or 401(k). That in itself is worth a celebration after many decades of hard work. You might also opt to collect your social security benefits, but it is generally advisable to wait until you reach full retirement age
Homestead benefits and property tax exemptions are a considerable benefit for those who already own or plan to own a home or property. Benefits vary by state, so you will need to see what you can qualify for where you live. Your local comptrollers’ office can provide information about offers regarding homestead benefits. For property tax exemptions, you must contact your local comptroller or tax assessor’s office for exemption information.
There is a lot to discover, learn, and know about how to proceed in life at age 65 and beyond. With Social Security benefit determinations, health insurance policies, and legal documents in order, you can begin to enjoy being 65. Start your education about being 65 or more today. Stay vibrant and healthy and enjoy those things you dreamed of doing when you were your younger self.
If you have any questions or need guidance in your planning or planning for a loved one, please don’t hesitate to contact any of our five offices by calling (443) 393-7696.
Bacteria May Cause More Diseases Than You Think

Health experts have been advising people for years about unhealthy habits being the cause of “lifestyle” diseases that are increasing across the US. These lifestyle diseases become more common with age and include heart disease, type 2 diabetes, some cancers, and Alzheimer’s disease. Around the globe, these diseases account for 70 percent of all deaths. New Scientist magazine is reporting evidence suggesting bacteria are to blame for the diseases and that this finding will herald the coming of a revolution in medicine.
However, don’t stop healthy habits just yet; findings in disease after disease indicate that bacteria are covertly involved which complicates the problem. Bacteria will invade bodily organs and then co-opt the immune system in a sort of parasitic relationship as the bacteria boosts their survival while making the human body break down. In theory, if the bacteria microbes can be stopped, there is a potential to defeat disease conditions like heart attacks or Alzheimer’s.
How can such an all-encompassing and seemingly simple underlying cause be overlooked for decades? Bacteria have eluded scientists because they work very slowly. Like a terrorist sleeper cell, the bacteria can hide or lay dormant for long periods inside of cells, and that makes them difficult to grow as a culture. DNA sequencing informs scientists and researchers that bacteria are in places they were never known or supposed to be and shaping the body’s inflammation responses.
The medical community is up-ended by this startling paradigm shift in disease causation. The information is so contrary to the current medical understanding that some scientists and researchers are only cautiously optimistic. Many scientists have spent years looking for answers to the root cause of diseases and are left frustrated by their inability to identify the reasons.
The worst offenders in the link between bacteria and disease are gum diseases. So it is bacteria that cause gum disease that is responsible for the most widespread disease of aging. Maurizio Tonetti of the University of Hong Kong calls gum disease “the most prevalent disease of mankind.” Gum disease is prevalent in 60 percent of Americans aged 65 or more. Germ theory finds the bacterial culprit known as Porphyromonas gingivalis (P. gingivalis) is linked to the broadest array of disease conditions.

Source New Scientist August 10-16, 2019


Source New Scientist August 10-16, 2019
Gum disease is releasing bacterial P. gingivalis into your bloodstream and promoting inflammation long before an infected tooth falls out. Americans 30 and older have a 43 percent rate of some form of gum disease, and many find dental insurance an added expense they didn’t think worth the price. What a price it turns out to be. Since bacteria cause diseases and bacteria are prevalent in the majority of Americans, what can be done to manage the role of these bacteria within the body’s immune system?
Some companies are developing drugs that will block specific inflammatory signals or responses to slow disease progression. Even if the goal to prevent a limited number of signals or responses is successful, it is unclear what tampering with the human immune system can unleash. While being a relatively simple identification with the advent of DNA sequencing, bacteria still manages to host itself in the body’s vastly complex immune system. This situation makes for a complicated fix.
Once P. gingivalis enters the bloodstream, it changes its surface protein. This change allows the bacteria to cloak itself inside the immune system’s white blood cells. Even within the cells themselves, they enter into its lining arteries. Here it can remain dormant and primarily undetected until it wakes to invade a new cell. Because bacteria are so hidden, antibiotics will not identify it to kill it, and immune defenses do not respond to it. There is much to consider from research and experimental perspectives.
Understanding the underlying cause of many diseases is a breakthrough, but an application for preventing disease based on this information is still in the developing stages. While the future does look brighter, it is always a good idea to live an overall healthy lifestyle.
If you have questions or would like to schedule a time to discuss your planning needs, please don’t hesitate to contact any of our five offices in Maryland by calling us at (443) 393-7696.
Elderly Parent Care Roadmap

Aging is something you cannot escape, and it affects all family systems. It can be challenging for adult children to imagine their parents as seniors and to understand and respond to the reality that each parent will age differently. Even if you are in the fortunate circumstance where your aging parents can go it alone for a long time there will come a day when assistance or long term care will be needed. There are things to consider as you help your parents live their best possible aging scenario. Managing their welfare takes time, research, and planning.
Your parents and their abilities to remain independent are most easily defined by activities of daily living and instrumental activities of daily living (ADLs and IADLs). Activities of daily living address daily functional mobility like getting in and out of bed or a chair, self-feeding, bathing and personal hygiene, the ability to use the toilet, and the ability to get dressed. These are essential daily living requirements that promote dignity and physical as well as emotional well- being for your elderly parents. If your parents are having difficulty managing these ADLs, it is an appropriate time to find help for them whether it is you or another qualified caregiver.
IADLs include all ADL activities and more. The additions are grocery shopping and cooking, medication management, laundry, and other housework, bill paying and finance management, using a telephone, and driving or using public transportation. Recognizing your parent’s limitations in any of these categories is a sign that you need to develop a care plan that provides appropriate assistance. The degree of change or sometimes multiple changes is an indication that staying at home may no longer be appropriate and safe for your parents. If you require assistance in determining suitable care needs, you can set up a comprehensive geriatric assessment by a medical professional. Take an honest look at the stage of life your parent is experiencing and then find the support and help they require.
Your aging parents’ geographical location is critical to consider as a family. Families are fortunate when one adult child lives nearby and can ensure their parent’s well-being. Video chat either online or through a phone application is one way to daily check on a parent. A friend may live close by and can do wellness checks and provide information about behavioral or health changes. If none of these options are viable, it may be time to discuss the idea of your parent(s) downsizing into another more supportive location and living arrangement.
Having this discussion is best before a parent’s adverse health event. Making residential changes without a previous plan in place can negatively impact on the parent, especially when experiencing a health care crisis. When aging at home cannot be appropriately managed, it is time to consider the alternatives. These alternatives may include independent living communities, assisted living communities, nursing homes, or living with a trustworthy and capable relative or family member.
All of these assessments and changes in your parents’ lives impact their financial outlook. Making necessary residential changes can often be very costly, and your parents may need additional financial support from government or community programs to offset the difference in expenses. It is critical to take advantage of all possible financial help. As an adult child, you may have to begin managing their finances and retirement funds more actively. There are various federal, state, and non-profit groups that provide free tax assistance for seniors.
Some of the better organizations to help you navigate what is available are online and include Benefits.gov, Area Agency on Aging, and Benefitscheckup.org. These groups can help you assess the best strategies for housing, healthcare, financial assistance, legal aid, transportation, in-home care services, prescription drugs, energy and utility support, and nutrition. BenefitsCheckUp is part of the National Council on Aging and is considered the nation’s most comprehensive online service for seniors with limited income and resources. The information available canvases all 50 states and the District of Columbia.
Caring for your aging parents should not be the job of one family member. The commitment should not be a burden, and responsibilities should be shared. Look for caregiver support organizations and forums as well as involving all family members. Everyone should do their part. The goal is to find the best blend of options and resources to allow your parents to age happily and well. Your parents’ health changes require that programs and opportunities change too. Caring for your aging parent is a dynamic process that must be retooled as their needs change.
We help families who are trying to navigate the maze of long term care either for themselves or for an aging parent. Please contact any one of our five offices by calling (443) 393-7696 so we can discuss your particular needs.
Don’t Fall for These Genetic Testing Scams

An alert has been issued by the US Department of Health and Human Services Office of Inspector General about a fraud scheme that involves genetic testing. The warning is for Medicare beneficiaries across the nation, and the federal government is working with law enforcement to put an end to the schemes. Already charges against 35 individuals have been brought for their alleged participation in healthcare fraud that accounts for 2.1 billion dollars in losses nationwide. The scam is perpetrated on the Medicare system at large and individual level.
First, the “recruiters” or “marketers” bogusly involve themselves with their targeted Medicare seniors. Typically, the scammer targets the victim through door-to-door visits, telemarketing calls, and booths at public events or health fairs. Some schemes even target retirement communities, offering free ice cream sundaes or gift cards to learn about this fantastic new genetic testing technology.
The deception begins with the offer of “free” screening, testing kit sent to your home via the mail, or an onsite cheek swab for genetic testing followed by obtaining the person’s Medicare information for fraudulent billing activity or identity theft. If the scam artist (“recruiter”) is working with an unethical doctor, they will pay that doctor a kickback in exchange for ordering the test. Once the lab processes the test, Medicare will reimburse the lab, and the lab then shares the proceeds of that reimbursement with the scammer. Genetic testing fraud occurs when an analysis or screening is performed but not ordered by a Medicare beneficiary’s treating physician and not considered medically necessary. If Medicare denies the claim, the recipient who permitted the screening becomes responsible for the entire cost of the test. The average price of personal genetic analysis ranges from 9,000 to 11,000 dollars.
Examples of genetic testing fraud can include, but are not limited to, the following screenings or tests:
- Cancer and hereditary cancer
- DNA
- Dementia
- Parkinson’s
- Pharmacogenomics or medication metabolization
What is the best way to avoid the genetic testing scam? If you receive a genetic testing kit in the mail, do not accept it unless you are sure your physician ordered it. Make certain it is sent from the doctor-approved company before opening it. If your physician did not order the test, refuse the delivery of it or return it unopened to the sender while keeping a record of the sender’s name and the date the item was returned. You can also report the sender’s information directly to the HHS OIG Hotline. Be skeptical of anyone offering a free genetic testing kit in exchange for providing your Medicare number. Once they have your Medicare data, it is easy for a scammer to compromise your data in additional fraud schemes. Guard your Medicare information, and if anyone other than your physician’s office is requesting your Medicare number, do not provide it. Medicare has a fraud hotline, and if you suspect you are a target, report the incident immediately. Again, you can report or submit a complaint to the HHS OIG Hotline.
Be sure to always review your Medicare Summary Notice (MSN) or Explanation of Benefits (EOB). Certain words or phrases indicate a questionable genetic test may have been completed. Words like laboratory, molecular pathology, and gene analysis are suspect and may indicate fraud, which you should immediately report as a billing error or possible fraud to your Senior Medicare Patrol (SMP) or the Health and Human Services Hotline.
Genetic testing is a fantastic tool made possible by scientific advancement, human genome sequencing, and increased computing capabilities. Twenty-five years ago, obtaining personal genetic information was inconceivable, but today the data can be obtained with a saliva sample. The test can provide information about your ancestors and assess your disease risk. Because the tests are expensive, it did not take long for scam artists to find ways to extract illicit financial gains from Medicare and its beneficiaries. Be aware of how scam artists target you and your personal information to avoid being a victim.
If you have any questions or need guidance through a situation you or a loved one are going through, please don’t hesitate to contact any of our five offices by calling (443) 393-7696.
Are Seniors Being Over-Prescribed Medications?

According to the Centers for Disease Control and Prevention (CDC), heart disease in the US accounts for one in every four deaths or about 610,000 people. It is the leading cause of death for both men and women. And yet, mcknightsseniorliving.com is reporting that in the United States, Alzheimer’s disease deaths have increased by 123 percent while deaths from heart disease have decreased by 11 percent. Alzheimer’s is currently the sixth-leading cause of death in the US, and one of every three seniors dies with some form of dementia. These numbers should give the government, and the health care industry pause as the silver tsunami of baby boomers continues into retirement. Current projections of Alzheimer’s disease-associated costs could be as much as 1.1 trillion dollars.
Currently, Alzheimer’s disease has no cure, and there is little hope for a near term solution. One bright spot on the horizon is the application of precision medicine. Precision medicine essentially drops the “one-size” fits all treatment model. Instead, it customizes health solutions based on each individual’s unique situation using technology. This precision approach is increasingly moving into real-world clinical settings and meeting with success. The components of medical data needed for input include a patient’s genome, bio-specimens, medications, medical history, demographics, diet, and lifestyle. All of these elements play a role in the customization of a precision medicine health plan.
One company practicing precision medicine is uMethod. At umethod.com there is a program called RestoreU METHOD that blends diagnostic tests, cognitive assessment, and lifestyle review information and then tailors a specific plan for each patient. These patients are specifically suffering from mild cognitive impairment, mild dementia, or mild Alzheimer’s disease. A personalized precision medical plan leads to better outcomes for patients. Data from RestoreU Method Health’s clinical efforts are reporting a very promising 76 percent improvement of memory or at least a cessation of the patient’s decline in memory.
One analysis by uMethod studies indicates that participants were on average, taking 15 drugs (not related to Alzheimer’s). Many of those drugs were contributory factors to the patient’s cognitive decline. The technology, specifically artificial intelligence (AI), proved far better at identifying issues and adjusting medications accordingly. AI is faster and more accurate at identifying drug to drug and drug to genome interactions that may worsen symptoms of Alzheimer’s. A potential drug interaction is when two medications known to interact are concurrently prescribed whether or not an adverse event occurs. These drug interactions may very well provoke life-threatening consequences, especially in the case of an elderly, frail patient. Because many seniors have co-morbidities the risk of an adverse drug reaction (ADR) is substantially increased. Over the past decade, the use of multi-drug regimes among the elderly has risen tremendously, and thus, the increased need for technology to be able to assess their complex interactions reliably.
Processing big data about patients allows AI to apply medical knowledge to specific criteria and thoroughly and quickly present an array of medical solutions and plans. These plans are highly detailed for the attending physician but are simplified for the patient. As a patient’s symptoms change over time, updated data can be input, and AI can recommend therapy changes that best address a patient’s dementia issues.
Developing treatments and possible drug cures for Alzheimer’s and other forms of dementia are going to remain a challenge for the foreseeable future. Multiple prescription medication interactions may be causing more harm than good to patients as the incidence of Alzheimer’s related deaths continues to increase at an alarming rate. What are your strategies in the event you become diagnosed with cognition problems that may lead to some form of dementia? Typically, dementias have a long pre-clinical phase followed by mild, medium, and severe category assessments. Medical directives that are specifically designed to address dementia issues are available. Check into precision medicine and how it might become part of a dementia directive you would like to have.
Contact any of our five offices today by calling (443) 393-7696 and schedule an appointment to discuss how we can help you with your planning.
Elder Abuse Recognition and Reporting

What is Elder Abuse?
Elder abuse is a problem that takes many forms. Unfortunately, many seniors are subjected to elder abuse and often times the abuse goes unreported and the abuser goes unpunished. Elder abuse may take the form of physical abuse, including hitting, striking, beating, kicking, and using excessive force. This may also include the overuse of restraints or drugs.
Emotional or psychological abuse is also a common form of elder abuse. This can be anything that causes emotional pain or distress and may include verbal assaults, intimidation, isolation, humiliation, and harassment.
Neglect is also a common form of abuse in senior citizens. Neglect is when a caregiver fails to provide the necessary care for the senior citizen under their care. In contrast, self-neglect is when a senior citizen who is mentally competent refuses to care for their own needs and causes harm to themselves.
Financial exploitation is yet another form of elder abuse. Financial exploitation is often committed by family members (most common), caregivers, or strangers.
Reporting Suspected Abuse
Adult Protective Services (APS) is often the first to receive reports of or to respond to reports of elder abuse. Their job is to provide for the safety, health, and well-being of elderly and vulnerable adults. The law requires those who work with senior citizens in various capacities to report to APS if they suspect elder abuse. When APS receives reports of abuse or neglect, they have several possible actions or interventions. They are responsible for receiving and investigating reports of elder abuse. They then must evaluate the victim’s risks and assess the victim’s ability to understand their risk and give informed consent. The APS worker can then develop a case plan for the abused elder. Once a case plan has been decided, the case worker can arrange for necessary care, medical attention, and legal consultation. Once this is done Adult Protective Services then monitors the services and evaluates the case.
More serious cases of abuse may be reported directly to the police. If a senior is in immediate danger, this may be the best course of action.
Many websites provide information on warning signs of potential physical abuse, emotional/psychological abuse, sexual abuse, neglect, and financial abuse. If you have a loved one who is a senior citizen, it is important to know the warning signs for abuse. It is also key to stay involved with the caregivers and to make regular visits to check on the care of your senior loved one. The National Adult Protective Services Association has important information on different types of abuse, as well as ways to get help in any state
If you have any questions about something you have read or would like additional information, please feel free to contact any of our five Maryland offices by clicking here to send us a message or by calling (443) 393-7696.
By: Jill Rosner, R.N., B.S.N. – Guest Contributor – Rosner Healthcare Navigation

On June 15, the World Health Organization (WHO) acknowledged Elder Abuse Awareness Day. Communities across the world participated in activities to bring awareness to a problem that faces many elders and oftentimes goes unnoticed. I share information about elder abuse every year to bring awareness to our community and perhaps alert others to keep their eyes open to this growing problem.
The WHO has adopted the following definition of elder abuse: Elder abuse (also called “elder mistreatment,” “senior abuse,” “abuse in later life,” “abuse of older adults,” “abuse of older women,” and “abuse of older men”) is “a single, or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust, which causes harm or distress to an older person.”
The key words “any relationship where there is an element of trust” are particularly important. A person or persons known to the elder commit most elder abuse.
Elder abuse may present in various ways and unfortunately is on the rise. Abuse may manifest in one or more aspects such as physical, emotional/psychological, sexual or financial. The National Adult Protective Services Association provides a list of the most reported types of abuse:
- Physical abuse: may include slapping, hitting, beating, bruising or causing someone physical pain, injury or suffering. This also could include confining an adult against his/her will, such as locking someone in a room or tying him/her to furniture.
- Emotional abuse: involves creating emotional pain, distress or anguish through the use of threats, intimidation or humiliation. This includes insults, yelling or threats of harm and/or isolation, or non-verbal actions such as throwing objects or glaring to project fear and/or intimidation.
- Neglect: includes failures by individuals to support the physical, emotional and social needs of adults dependent on others for their primary care. Neglect can take the form of withholding food, medications or access to health care professionals.
- Isolation: involves restricting visits from family and friends or preventing contact via telephone or mail correspondence.
- Financial or material exploitation: includes the misuse, mishandling or exploitation of property, possessions or assets of adults. Also includes using another’s assets without consent, under false pretense, or through coercion and/or manipulation.
- Abandonment: involves desertion by anyone who assumed caregiving responsibilities for an adult.
- Sexual abuse: includes physical force, threats or coercion to facilitate non-consensual touching, fondling, intercourse or other sexual activities. This is particularly true with vulnerable adults who are unable to give consent or comprehend the nature of these actions.
- Self-neglect: involves seniors or adults with disabilities who fail to meet their own essential physical, psychological or social needs, which threatens their health, safety and well-being. This includes failure to provide adequate food, clothing, shelter and health care for one’s own needs.
Abuse and exploitation can be committed by spouses, family members, formal caregivers in the home or in assisted living housing or nursing homes or strangers who prey on the aging population among others who may be trusted friends or acquaintances.
It can be argued that the exploitation of elders that comes in the form of constant barrages of requests from charities, phone solicitation for products to aid a senior and marketing to seniors can also be perceived as a trusted source. It seems as though as soon as the golden age of retirement approaches seniors receive constant and unyielding piles of mail and calls to donate, buy or participate in some way. We must all be very judicious and diligent to protect ourselves from the predators that exploit the older population.
The statement “if you see something, say something” is a perfect reminder that minding your own business is not always the soundest advice. Elder abuse is oftentimes noticed by neighbors, bank employees, family members, friends and acquaintances and either denied or ignored because people don’t want to get involved or “stick their noses in.” Trust me, if we all paid attention to the warning signs, the true extent of the problem would finally be appreciated. There is much work to be done to strengthen laws, increase and enforce punishment for this serious crime.
I remind the banking industry, there is a mandatory reporting law that you must report any suspicious activity such as someone bringing a customer to the bank and changing their accounts, any suspicion of undue influence to pressure or coerce one to make changes to accounts, withdrawals or moving money. This applies to those who may seem competent to you but may seem to be told what to do and those who you may have noticed odd behaviors over time.
Those suffering from even the earliest effects of some type of dementia become preoccupied with their accounts and may come into the bank or call frequently to “check” on their accounts and balances. They may make repeated withdrawals. They may exhibit some paranoia about their accounts being tampered with or having money stolen from them. This must be reported! I am personally fed up with banking personnel looking the other way and not knowing what to do. It is your responsibility to protect your customers from abusers and oftentimes from themselves if they clearly seem off or confused and constantly stressed about their accounts. Please report suspicious activity to Adult Protective Services (APS). Just a call can save an elder from abuse or misuse of their funds.
Jill Rosner is a registered nurse, certified aging life care manager and owner of Rosner Healthcare Navigation. She provides patient advocacy and care management services to clients with health and aging issues. Contact her at jillrosnerrn@aol.com or 410-591-6378.
By: Nicole T. Livingston, J.D. – Associate Attorney – nicole@elvilleassociates.com, 443-393-7696
Some clients are reluctant to share their planning with their family. You may feel the plan is private or needs to wait to be unveiled at the time of your death. Perhaps, you do not want to create tension if you chose one family member over another to act as your executor or power of attorney. Many may be uncomfortable bringing up the topic for fear of the reaction from family members. We have found by explaining your estate plan now and having regular meetings with your executor can prevent problems during the administration process. You can tackle difficult issues while you have an opportunity to express your thoughts and feelings. Waiting for the big reveal after your death can cause some families to break up and never speak to each other again.
A good way to start the discussion is to have a family meeting with your estate planning attorney and other advisors, such as your financial advisors and certified public accountant. At Elville and Associates, we encourage you to schedule this meeting with us. We can lead the discussion and bring up uncomfortable topics in a nonconfrontational style. Explaining how your plan works to your family members will allow them to understand why decisions were made and give them an opportunity to ask questions.
Start with a convenient time and location for family members to meet. Your attorney’s office is a good location because it conveys the seriousness of the discussion and allows for a clear beginning and end time. Allowing family members to participate and ask questions directly to the drafting attorney may clear up misperceptions they may have. This first step opens the door for more discussions in the future to be held in a less structured setting. During this meeting, no financial discussions of the size of your estate or specific values of your assets needs to be discussed. Instead, the meeting can explain the documents you have prepared and what the family can expect upon your death or if you become disabled.
Initially, there may be anxiety associated with the meeting due to sensitive issues that may be discussed. Planning involving a blended family or a beneficiary who may not be financially responsible to control the inheritance that you leave to him or her can be challenging. If trusts are involved, your attorney can explain why and how they are being used. Your values in creating the plan the way you did can be explained and understood by your family while you are living. No one wants to leave a mess behind and opening this discussion during a family meeting is a good first step to take to leave behind a legacy rather than a lawsuit.
You need to discuss with your health care agent your decisions for end of life care. During the estate planning process, you signed an Advance Medical Directive. The family meeting is an opportunity to discuss the decisions you made. If you allowed your agent to have flexibility, then explain what you intended this to mean. For example, you may have requested a feeding tube if you are unable to take enough nourishment by mouth. You can discuss with your agent for how long this may last. If the decision is made for you to enter hospice, let your agent know it is okay to discontinue the feeding tube. At some point, with a persistent vegetative state, a feeding tube may be prolonging your life with extraordinary medical bills. This may not be what you intended. You may have wanted a feeding tube for comfort and now it is a burden. It is difficult to document all the variables in a health care situation which is why it is important to have a discussion now about your health care.
Writing a statement about your goals and values and what is especially important to you during the last part of your life can alleviate stress and anxiety family members experience when trying to make final decisions regarding your life. You can locate this paragraph in Part II: Treatment Preferences (“Living Will”).
Part III of your Advance Medical Directive allows you to state your wishes regarding your funeral and burial arrangements. You may have decided who should make decisions about the disposition of your body, but you may not have discussed with them what you desire. Some funerals involve many decisions that are like planning a wedding; however, the time frame is much shorter – often having to plan everything within a week or two. The decision of burial or cremation is only the beginning. Your agent may have to locate a church and decide on a ceremony. Or you may desire a memorial service with no religious affiliation. Decisions regarding gospel verses or specific bible readings and who will read them, songs and whether you want a choir or a specific soloist, and the type of church ceremony or memorial service and whether a casket or urn is present will all have to be decided quickly. After that a location for a repast might be required which involves food and beverage selections. Notifying friends and family may be challenging to handle alone and often involves coordination of travel and lodging arrangements. Decisions about flowers or donations in lieu of flowers to a specific charity can be challenging if family members do not agree. Often the task of writing an obituary falls on your agent. It can be contentious if family members all want to have input. You can alleviate some of this burden by discussing your wishes now.
One final thought – your agent needs to have access to these documents. Whether you join DocuBank to store your documents or you use a home safe, you need to inform your agent where the original documents are located and how to access the safe if you are placing your documents in one. Providing your agent with copies now is also a prudent decision. After signing your estate planning documents, you have some work to do to make sure that your wishes are properly followed. We feel a family meeting is the best first step to accomplish this task.
By: Stephen R. Elville, J.D., LL.M. — Principal

They say that if you simply hang around long enough you will likely see it all. This seems to be the case with one new law that was recently passed by the Maryland Legislature, the new elective share law (House Bill 99; Senate Bill 192), otherwise known among lawyers as the “augmented estate” or “new elective share” legislation. This legislation “hung around” for the past several years and finally will become law (effective October 2020). Here is a brief history.
Under present (still currently existing) Maryland law, a surviving spouse was entitled to elect against the will of his or her deceased spouse to receive one-third (1/3) if there was surviving issue of the decedent, or one-half (1/2) if there were no surviving issue of the decedent, of the “net estate” – basically the net amount of the probate estate. This meant that a spouse with bad intentions could disinherit the surviving spouse by up to two-thirds (2/3) and the surviving spouse could only exercise a right of election over the limited statutory amount of the net probate assets described above. Unfortunately for the aggrieved spouse, this also meant that he or she (likely she) had no right of election over assets owned by the deceased spouse that passed outside of probate (passed via non-probate transfer) such as joint accounts, transfer on death designations (TOD), payable on death designations (POD), beneficiary designations (IRAs, Qualified Plans, and life insurance), and real property passing by life estate deed. As a result, a spouse with bad intentions could disinherit a surviving spouse by sixty-six and two-thirds percent (66 2/3%) of the net probate assets, and one hundred percent (100%) of non-probate assets.
Then, beginning in 1990 and leading up to 2008, two cases Knell v. Price, 318 MD. 501; 569 A.2d 636 (1990), and Karsenty v. Schoukroun, 406 MD 469; 959 A.2d 1148 (2008) changed the status quo, but did not move the needle enough to give a surviving spouse meaningful rights to non-probate property to which they were arguably entitled. Although a full analysis of these cases is beyond the scope of this article, they stand for the proposition that a surviving spouse is entitled to an elective share over an estate broader than the probate estate – an augmented estate that includes not only the traditional net probate estate but also the non-probate assets of the decedent spouse. These cases, especially the latter, established certain tests, approaches, and factors by which a court could determine whether the nonprobate assets of the decedent would be subject to the elective share of the surviving spouse. Although these cases represented progress, an aggrieved surviving spouse nonetheless remained in a situation of great legal uncertainty and disadvantage, considering that more likely than not she would have to engage in costly and protracted litigation to prevail on the issue of electing against the augmented estate of the deceased spouse.
With the passage of the new elective share law, the Registers of Wills and the Courts will take a formulaic approach designed to bring sensibility and fairness to this complex issue, for both spousal and non-spousal beneficiaries. This will most likely be a difficult and arduous process for all parties involved, especially after implementation in 2020. Since most traditional couples – couples where the union was a first marriage and children from that first marriage exist – leave assets for the benefit of the surviving spouse either outright or in further trust, and the non-probate assets of the deceased spouse usually flow by beneficiary designation to the surviving spouse, the new elective share law will have little or no impact those couples. However, and there are many examples too broad in scope to discuss here, two main categories of surviving spouses will be impacted the most, as follows: (1) the second (or more) marriage surviving spouse with or without children of their own; and (2) the disabled surviving spouse.
The surviving spouse in a second, third, or more marriage who has been disinherited by their deceased spouse, usually because he or she has children of their own or other relatives to whom they intend to leave assets at their death (the death of the first spouse to die), will be impacted by the new law. Furthermore, it is important to note that even more impact will inure to the deceased spouse and his or her children because of the new law. The reason is simple – under the new elective share law, where an uninformed spouse in a second or more marriage who with or without the mutual agreement of their spouse leaves assets to their children or other relatives, a very common occurrence), the surviving spouse may thwart the estate plan of the deceased spouse by electing against the probate and non-probate assets of the decedent. This situation may only be legally avoided through the use of pre-nuptial or post-nuptial agreements that specify the waiver of the surviving spouse’s right to a spousal elective share.
Spouses who die leaving a disabled spouse will fare better, and the new elective share law allows for the placement of the surviving spouse’s elective share amount into a testamentary special needs trust (a common practice among elder law attorneys) without exposing that statutory elective share amount to the claims of Medical Assistance. This carve-out exception means that elder care planning for spouses where one spouse has an impairment or other disability can continue unabated – a happy result for the benefit of couples who wish to be proactive under circumstances where choices otherwise seem very limited and where long-term care costs continue to devastate family finances.
In summary, the new elective share law which had previously confounded lawmakers, the Registers of Wills, and others for several years is now the law in Maryland effective next fall (fall 2020). Those persons who plan to disinherit their spouses for bad-intentioned purposes (likely very few), or remarried spouses who plan to leave assets to their children from a prior marriage should they be the first spouse to die (in the new marriage), should take notice of this new game-changing law. Pre-nuptial and post-nuptial agreements, already important asset protection planning tools in and of themselves, will now take center stage as a first and preeminent step in estate planning for many couples, and an important point of client education for all.