Do you get upset, angry, or cry easily? Tips are here!
How often do you feel like crying?
Do you cry or get upset with the slightest provocation?
Do things that were manageable before now seem overwhelming?
How is your stress level?
Can you handle one more piece of bad news?
If you find these questions challenging (or you think I’ve been spying on you), please know you are not alone. Throughout the globe mental health has taken a hard hit. There are many indicators that each person has struggled more than usual in the past two years.
Managing Your Emotions with Sleep
One of the key factors of managing your emotions is good deep sleep. Sleep, anxiety, and pain are closely linked. Anxiety makes pain feel worse. Pain and anxiety both make it difficult to sleep. Poor sleep makes it difficult to manage anxiety or pain. Sleep is where I have seen the most people break this difficult cycle.
And rarely is medication the way to achieve that kind of restorative sleep. Sleep medications alter the types and depth of sleep you get so rarely do medications, alcohol, or other substances help you feel truly rested in the morning.
So, what can you do? There are several steps you can take for more natural effective sleep. These are often called sleep hygiene. Consider which of these you could add or improve.
Better Sleep Techniques
- Keep your sleep and wake times as regular as you can. I know this can be difficult but if you can, avoid wide variations.
- Leave the screens behind. Ideally stop looking at screens an hour or more before going to bed. And keep them away from your bed. If you need the alarm, use the feature that will keep it silent until time for the alarm.
- Have a wind-down routine. Let your brain and your body know you are getting ready to sleep.
- Make sure to get good movement during the day to differentiate awake from sleep times. Time outdoors and in nature can lower stress, anxiety, irritability, and blood pressure. It can increase endorphins and dopamine to help you feel more positive.
- Do what you find relaxing. A warm bath or shower, gentle stretching, soft music, lavender or other scents you like, and other relaxation techniques can help you calm and relax.
- Use sounds to diminish distraction from a snoring partner or other noises. You can search online for white noise, pink noise, brown noise, rain sounds, ocean sounds, or nature sounds.
- Quiet your mind. One way to do this is deep breathing slowly in and out. Either count slowly in through your nose and out through pursed lips (as if around a straw) or recite a favorite quote or verse while breathing. You can also look for many options for meditation.
- Avoid or minimize length of naps. Too much sleeping during the day will disrupt sleep at night.
- Keep your bed for only sleep and sex. Watching television or studying in bed then trying to sleep can minimize your chances to fall asleep easily and get good sleep.
- If you wake up during the night or have trouble getting to sleep, go back to the breathing to help quiet your mind. If pain is keeping you awake, try gentle stretching then go back to bed.
Use whatever combinations of strategies that work best for you. Of course, another key factor is to get enough sleep. I know several successful people who deprive themselves of sleep in order to obtain a few more hours to work. On rare occasion when up against a big deadline, that is not so detrimental (unless you are driving tired.). Otherwise, this has many long-term negative health effects. Too little sleep increases risk of high blood pressure, heart attack, and stroke among other effects.
Next Steps
Controlling your emotions is just one of many positive benefits to taking time and effort to sleep better.
If you would like to know more:
Retirement Wellness Strategies is an exclusive one-on-one process with a professional expert guide. (www.retirewellness.com)
Propel Comprehensive Wellness is a self-guided online monthly subscription way to gain the tools you need to thrive for a lifetime. (www.propelyourwellness.com)
Unsure? Schedule a time for us to talk: https://calendly.com/retirewellness/20-minute-free-inquiry-call
Dr. Michellle Fritsch is an author, nationally renowned speaker, and founder of Retirement Wellness Strategies. You can call her at 410-472-5078, email her at michell@retirementwellness. com, or visit her website at www. retirewellness.com.

Serving as a trustee of a trust can be a huge responsibility, so trustees are entitled to compensation for their work. The amount of trustee compensation depends on the type of trustee and the complexity of the trust.
Depending on the trust, a trustee’s duties can include managing trust assets, making distributions to beneficiaries, paying taxes, and creating an annual report of all income and distributions. Performing these tasks can involve a lot of work, so it makes sense that trustees are compensated for their time.
The terms of the trust may explain exactly what trustee compensation is appropriate, but many trusts don’t provide specifics. With no guidance from the trust document, the laws in most states usually require that trustee compensation be “reasonable,” without giving more details. What is considered reasonable is going to depend on the type of trust. Things to consider include the following:
- The amount of time needed to administer the trust.
- The complexity of the trust.
- How many beneficiaries are involved.
- What type of assets need to be managed.
Often family members and friends serve as trustees without trustee compensation. If their duties are modest — simply distributing trust assets, for example — that might be fine.
With a more complicated trust, however, some trustee compensation is expected. Professionals usually charge an annual fee of between 1 percent to 2 percent of assets in the trust. So, for example, the annual fee for a trust holding $1 million could be between $10,000 and $20,000. Often, professionals charge a higher percentage of smaller trusts and a lower percentage of larger trusts.
A non-professional trustee usually charges less than a professional. However, if the non-professional trustee is doing all of the work for a trust, including investments, distributions and accounting, it may be appropriate to charge a similar fee. On the other hand, if the non-professional trustee is paying others to perform these functions or is acting as co-trustee with a professional trustee, charging this much may be seen as inappropriate. A typical fee might be a quarter of what the professional trustee charges, or .25 percent (often referred to by financial professionals as 25 basis points). If taking a percentage of the trust assets would deplete the trust, non-professional trustees may also charge an hourly rate for their work.
In addition to compensation for their work, trustees are also entitled to reimbursement for any expenses that they might incur in the course of performing their duties, including travel, storage, insurance, or taxes.
If the beneficiaries are unhappy with the trustee compensation received, they can challenge it in court. And if trustees think they are entitled to more trustee compensation, they can also appeal to court to receive higher payment.
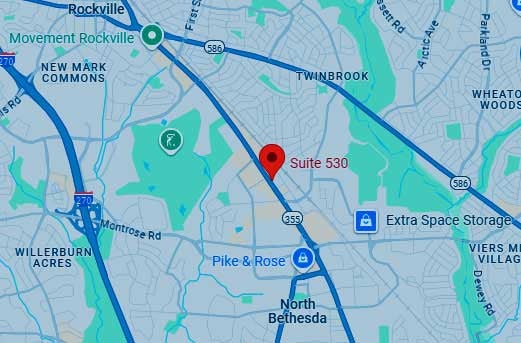
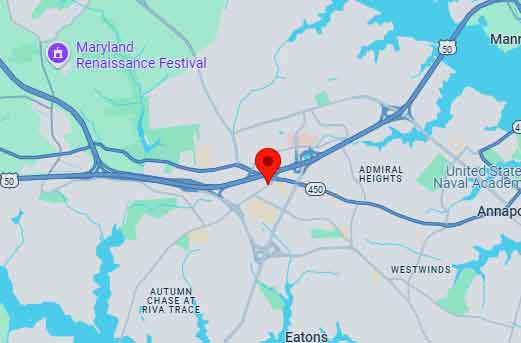
Whether you are setting up a trust or have been appointed trustee and want to know what trustee compensation is reasonable, consult with the estate planning attorney at Elville and Associates. Our attorneys are well-versed in addressing all matters involving trustees, including choosing the right one for your situation, counseling trustees regarding their duties and responsibilities, as well as acting as trustee in certain situations. To set a time to speak with an attorney about this subject, please contact the firm’s Executive Assistant, Mary Guay Kramer, at mary@elvilleassociates.com, or at 443-741-3635. Or, you may fill out a contact form online and we’ll respond to you promptly.
To view Elville and Associates most recent webinar titled, “Trustee Selection – How to Choose the Right One for You” please click here.
#elvilleeducation
#elvillewebinarseries
Watch our firm’s introductory video here!
More Webinars from Elville and Associates
The education of clients and their families through counseling and superior legal-technical knowledge is the mission of Elville and Associates. We hold multiple educational events every month. Click to view our calendar of educational webinars and events or visit the Elville and Associates YouTube channel to view recordings of our past webinars.
#elvilleeducation #elvillewebinarseries
Not everyone wants to take the required minimum distributions from their retirement accounts right away. If you don’t want your IRA distribution, one option is to donate it to charity and get a tax deduction.
You are required to begin taking IRA distributions from your tax-deferred IRA when you reach age 72 (70 ½ if you turned 70 ½ in 2019 or before) even if you don’t need the money. The distributions are added to your income and taxed at the same rate, which could put you into a higher tax bracket, especially if you are still working.
If you don’t want the IRA distribution, you may want to consider donating the distribution directly to charity through a qualified charitable donation. By donating your required minimum distribution, the IRA distribution won’t be included in your gross income, which means lower taxes overall.
A qualified charitable donation can also be a good way to get a tax deduction after the 2017 tax law doubled the standard deduction, making it harder to get a deduction for a direct charitable contribution. If your charitable contributions along with any other itemized deductions are less than $12,950 a year (in 2022), the standard deduction will lower your tax bill more than itemizing your deductions, which can be a disincentive to donate to charity. A qualified charitable donation is a way to make a donation and receive a tax benefit from it.
In order for the donation to count as a required minimum distribution, the donation must be made directly from the IRA to the charity. Funds distributed directly to you do not count. The charity must be approved by the IRS, and different IRAs have different rules about how to make the distributions. If you make a qualified charitable donation, you cannot also itemize the deduction. The maximum amount you can donate is $100,000. If you donate less than your required minimum distribution, you will need to take the remainder as an IRA distribution.
For more information from the IRS about IRA distributions, click here. If you are charitably inclined and would like to learn more about different options to donate to charity based on your situation and goals, contact the attorneys at Elville and Associates to schedule a consultation today.
#elvilleeducation
Often-Overlooked Earned Income Tax Credit Expanded, Now Covers More People with Disabilities

For tax year 2021, the IRS is expanding eligibility for the earned income tax credit (EITC), an important antipoverty measure that assists those with low-incomes. One key impact of these changes is that more people without children, many of whom are also people with disabilities, will qualify. Traditionally people with disabilities have “left money on the table” by assuming they wouldn’t qualify for the EITC.
Here’s how it works: if you file taxes and your earned income is below a certain level, you can apply the earned income tax credit to the amount of federal taxes you owe. For many earned income tax credit recipients, the credit may not only result in paying no taxes, but in receiving a refund from the IRS.
“There are important changes to the earned income tax credit that will help this credit reach more hard-working families this year,” IRS Commissioner Chuck Rettig said in a statement. “We urge people potentially eligible for this valuable credit to review the guidelines; many people each year overlook this and leave money on the table.”
People with disabilities, especially those without children, have traditionally overlooked the earned income tax credit for various reasons. According to the IRS, many eligible people miss out on the EITC because they fall below the income threshold requiring them to file taxes, even though they can still file taxes and possibly get the credit. Others incorrectly believe that receiving the earned income tax credit will jeopardize their eligibility for other government benefits. Refunds received via the EITC are not considered income for the purposes of means-tested government benefit programs, such as Medicaid, Supplemental Security Income (SSI), Supplemental Nutritional Assistance Program (SNAP) benefits, Section 8 housing, or other programs with maximum income limits. In fact, income from SSI, Social Security Disability Insurance (SSDI), or military disability benefits is not considered “earned income” (see below for details).
Maximum Credit Triples
For tax year 2021, the earned income tax credit is available to individuals 19 years and older, without qualifying children and earning income up to $21,430. Married couples filing jointly qualify for EITC by earning up to 27,380. This limit goes up depending on the person’s tax filing status and the number of qualifying children in the person’s household. For a married couple filing jointly with three qualifying children, the maximum household income is $57,414. While in the past, the earned income tax credit was only available to people between the ages of 25 and 64, now senior citizens of any age can claim the credit if they have earned income.
Taxpayers may claim a child with a disability or a relative with a disability of any age to get the credit if the person meets all other EITC requirements. For 2021 only, the IRS has also lifted the child requirement, so that the maximum EITC for filers with no children is $1,502, almost three times more than the 2020 maximum of $538.
Here’s an example of how the credit might work for a single worker: John is 50 years old, single, and works part-time, earning $12,000 in 2021. This is just under the current income threshold required to file taxes, but if John does file and claims the EITC, he should receive a refund of $1,439, according to Tax Outreach’s Earned Income Tax Credit Estimator. If John earned $15,000 last year, he’ll be eligible for a $980 credit, according to the same estimator.
‘Earned Income’ Defined
What counts as earned income? This is a key question for people with disabilities, many of whom receive funds from several different sources.
Aside from wages, salaries, or tips, earned income includes earnings from work-for-hire contracts and self-employment, and payments from employer-provided disability benefits until the recipient reaches “minimum retirement age,” meaning the age the person could have begun receiving a pension or annuity from their former employer. Investment income is also a factor, although for 2021 only, the IRS is capping this at $10,000. So if your earned income falls below the threshold, and you can also claim less than $10,000 in interest and gains on your investments, you could still qualify for the EITC program.
It’s just as important to note what doesn’t count as earned income. This includes Social Security, pensions and annuities, unemployment insurance, EITC refunds, and income from such government benefits programs as SSDI, SSI, and military disability benefits. In addition, disability income claims from a private insurance policy, in which the individual pays the premium, is not considered earned income.
If you think you might qualify for the earned income tax credit, especially if you or a family member has a disability, it pays to look over the IRS changes carefully as you prepare your tax return for 2021. And it can’t hurt!
For people needing assistance in filing their taxes, the IRS has a Volunteer Income Assistance Program, which provides free services for certain people making less than $58,000, including people with disabilities and limited English speakers. For the elderly, the IRS has a similar program, known as the Tax Counseling for the Elderly program.
For the IRS’s recent update on the program, including a link to a YouTube video on how the EITC can put more money in your pocket, click here.
The attorneys at Elville and Associates are well-versed in tax planning and estate planning for individual and families through our “caring for clients” model that focuses on client education, collaboration with financial planners, CPAs and other professionals, and compassion. Contact the attorneys at Elville and Associates today to set a free consultation to discuss how we can help you start planning for your life and planning for your future legacy. To set a time to meet with us, click here. We look forward to meeting you!
For an introduction to Elville and Associates, click here to view our new firm introductory video!
More Webinars from Elville and Associates
The education of clients and their families through counseling and superior legal-technical knowledge is the mission of Elville and Associates. We hold multiple educational events every month. Click to view our calendar of educational webinars and events or visit the Elville and Associates YouTube channel to view recordings of our past webinars.
Putting It All Together – A Diagnosis to Adulthood Guide of Navigating the Disability World
Elville and Associates welcomes back guest presenter Eric Jorgensen, a Special Needs Advisor with Special Needs Navigator who provides a complete timeline overview of what families and the professionals they work with can expect from the original diagnosis until the child survives the parents. Eric highlights key times when specific planning items such as completing an estate plan, getting life insurance, or applying for SSI should be completed. He also discusses potentially lesser-known resources such as Low Intensity Support Services and Pre-Employment Transition Services.
Key takeaways include:
– Life insurance, ABLE accounts and Special Needs Trusts are critical tools, but not the plan
– Don’t wait until your child is in the last year of school to think about his or her transition
– You are not applying for benefits for you – delaying because it doesn’t seem worth the effort could be sabotaging your child
More Webinars from Elville and Associates
The education of clients and their families through counseling and superior legal-technical knowledge is the mission of Elville and Associates. We hold multiple educational events every month. Click to view our calendar of educational webinars and events or visit the Elville and Associates YouTube channel to view recordings of our past webinars.

While it is preferable to conduct long-term care planning well in advance of needing care, if you haven’t planned ahead, there are some strategies available to avoid spending all your assets. Three so-called “half a loaf” approaches allow a Medicaid applicant to give away some assets while still qualifying for Medicaid.
In order to be eligible for Medicaid benefits a nursing home resident may have no more than $2,000 in “countable” assets (the figure may be somewhat higher in some states) in addition to the home, and the resident cannot have recently transferred assets. (A spouse living at home may keep more.)
Congress has imposed a penalty on people who transfer assets without receiving fair value in return. This penalty is a period of time during which the person transferring the assets will be ineligible for Medicaid. The penalty period does not begin until the person making the transfer has (1) moved to a nursing home, (2) spent down to the asset limit for Medicaid eligibility, (3) applied for Medicaid coverage, and (4) been approved for coverage but for the transfer.
If a Medicaid applicant has excess assets, he or she must spend down those assets in order to qualify for Medicaid. However, Medicaid applicants who want to preserve some assets have a few options:
- Gift and cure. The nursing home resident transfers all of his or her funds to the resident’s children (or other family members) and applies for Medicaid, receiving a long ineligibility period. After the Medicaid application has been filed, the children return half the transferred funds, thus “curing” half of the ineligibility period and giving the nursing home resident the funds he or she needs to pay for care until the remaining penalty period expires.
- Promissory note. The nursing home resident gives half of his or her funds to the resident’s children (or other family members) and lends them the other half under a promissory note that meets certain requirements in the Medicaid law. The resident uses monthly repayments of the loan, along with his or her income, to pay nursing home costs during the penalty period.
- Annuity. The nursing home resident gives half of his or her funds to the resident’s children (or other family members) and uses the remaining assets to buy an immediate annuity. In most states the purchase of an annuity is not considered a transfer that would make the purchaser ineligible for Medicaid. Income from the annuity can be used to help pay for long-term care during the Medicaid penalty period that results from the transfer. In such cases, the annuity is usually short-term, just long enough to cover the penalty period.
These “half a loaf” strategies may not work in every state and none of these “half a loaf” strategies should be attempted without the help of an attorney whose practice includes Medicaid planning.
The attorneys at Elville and Associates are well-versed in Medicaid planning along with the above-mentioned “half a loaf” strategies. Contact us to set a time to discuss if this strategy would benefit you.
#elvilleeducation
By: Allyson Stanton, LBSW, ALCP, Geriatric Care Manager and Owner of Stanton Aging Solutions
For those of us with aging parents, the time will come when we have to discuss sensitive issues, such as where they will live, who will make medical decisions, who will handle their finances and what their wishes are for their final resting place. You might be feeling nervous just starting to think about the answers.
I often wonder why we wait until they “age” or until they hit a particular birthday. Instead of thinking, “My dad is 85 years old, so now is the time to talk,” change your mindset to, “The time is now, and it has nothing to do with age.” The same goes for waiting until a parent starts to decline mentally or have other health challenges. By then it may be too late for them to make well thought out decisions, or it’s a far too sensitive time to start asking these tough questions. Timing is important.
Give Your Parent a Voice
When talking with loved ones, make the conversation about empowerment. Show them that you want to know how they feel and what they think so that you can honor their wishes. I like to refer to it as “aging life goals.” How do they see themselves five, 10, and even 15 years from now? One way to open this conversation is to share that you have been thinking about this for yourself. If you haven’t, then putting documents in place and sharing your wishes with your own children is something you and your parents can do together.
Listen Without Judgement
We all have preferences in what we imagine our older years will be like, and it is not about what we think is right or wrong. This isn’t the time to judge, but simply start the discussion and listen. A conversation starter could be, “Are there things that are really important to you that you want me to know?” and follow up with, “What do you not want?”
Set Your Ego Aside
You may think you are the best person to make these decisions, but it should be a family discussion. Because of my career, it’s not surprising that my gut reaction would be for me to talk to my mom about this and handle everything. However, my sister is a nurse and my brother is good with finances. Let your family know in advance that you’d like to talk about this. Call a family meeting. Feelings can get hurt when the family hasn’t thought through this before, or your parent could feel pressured. Sometimes revelations arise when parents have already decided on their representative but haven’t shared it with anyone — even the child.
So as hard as it is to put your ego aside, it is necessary for an honest conversation. Maybe one sibling or two should be the Medical POA/Health Care Agents, and another sibling can be the Financial POA. In any case, it should be someone who your parent trusts. The decision is theirs.
Do Some Research First
Before the discussion, you and other family members should prepare. Instead of presenting only the challenges of making these life decisions, be prepared to offer options. There are Aging Life Care Professionals, like us, who can begin to educate you about residential facilities, budgeting, healthcare services and so much more. Your local Office on Aging, financial planners and elder law attorneys can also provide guidance and support. We’re pleased to offer referrals from our trusted network.
Please reach out to us at help@stantonagingsolutions.com or call us at (443) 812-1028.
By Allyson Stanton, LBSW, ALCP, geriatric care manager and owner of Stanton Aging Solutions www.stantonagingsolutions.com

By: Ellen S. Platt, MEd, CRC, CCM – President & Certified Aging Life Care Manager of The Option Group
For many people, gathering with family and friends is a time-honored tradition, strengthening bonds and creating (or reliving) joyous memories. Dementia presents many challenges in the everyday cycle of life, as daily routines and the avoidance of stressful situations is preferable.
However, the question presents itself: is safe travel possible for the person with dementia? Let’s keep in mind that having dementia doesn’t automatically preclude traveling with a family member or trusted caregiver. However, a serious assessment of their symptoms makes sense before plans are finalized and put into action. Remember, there are too many obstacles and decisions to be made when traveling, so a person with dementia should never travel alone.
5 Tips to Consider in Trip Planning with a Person with Dementia
Take into consideration the following when thinking about planning a trip:
- Determining if Someone with Dementia Should Travel
•Consider the stage of dementia the person is in
•Identify their common symptoms and problems and if these could be obstacles during travel
- Benefits of Traveling for People with Dementia
•Many losses come with a dementia diagnosis, which often includes traveling
•Continuing to travel as long as the person is able, helps minimize losses that accompany the diagnosis
•Planning to travel with someone with dementia allows them and the caregiver to stay connected to friends and family
3. Preparing Before the Trip
•If flying, book trips during the least-busy times and board early
•Arrive a few days early so the person can adjust to the new environment
•Try and anticipate problems and emergencies, and prepare solutions or actions you will take •Talk to their doctor about medication to help with agitation
•If possible, avoid large crowds and noisy places
•Bring doorknob covers and locks to prevent wandering
•Advise airlines, hotels, and other agencies that you are traveling with someone with dementia so that they are aware of the situation and can help with any necessary accommodations •Research important locations near your destination, such as medical facilities and pharmacies •Bring important documents: doctors’ names and contact information, a list of medications and food/drug allergies, emergency contact information, insurance information, copies of legal papers
- Tips During the Trip
•The traveler with dementia should wear identification and have emergency contact information with them
•Maintain as normal of a schedule and routine as possible
•Bring familiar items such as pillows or blankets
•Avoid over-scheduling the trip with activities like sightseeing that may be overwhelming
- Additional Considerations
•If possible, stick with familiar destinations
•Have a backup plan in case plans change unexpectedly, which could include getting travel insurance
•Inform family, friends, and anyone the person with dementia will be interacting with of their diagnosis and what to expect
•Try to keep travel time short
•Set realistic expectations for the trip
To answer the earlier question, is safe travel possible for the person with dementia? As an advocate, use the above tips to seriously consider the benefits and risks of not only travel but the type of travel. Be prepared for the unexpected and limit the stress on both the individual and the travel companion. Enjoy the holiday season and make the most of life’s chances for engagement, health, and as always, safety! If you or someone you care about needs additional support, The Option Group is here to help. Please contact our professional care management team for assistance.
About Ellen Platt and The Option Group: Founded in 2010, The Option Group’s compassionate team of experienced Certified Life Care Managers serves families, their loved ones, medical professionals, and professional family advisors in Maryland, Pennsylvania, and Delaware. The firm understands the challenges of caring for an individual who needs assistance due to aging, dementia, disability, or serious illness.
Their skilled providers possess over 100 years of combined experience navigating the healthcare maze and accessing hundreds of quality resources. The Option Group helps families spend quality time with their loved ones, providing clear choices that lead to better care. For more information, visit www.theoptiongroup.net or call 410-667-0266 (MD) or 717-287- 9900 / 610-885-8899 (PA) / or 302-858-6449 (DE).